Written by Ophir Ronen
Alarm fatigue is a critical problem in ICUs worldwide and affects clinicians, patients, and caregivers.
Alarm Fatigue is the incessant noise emitted from vital signs devices in every room in every ICU. Nurses and Doctors miss alarms because they are overwhelmed by the cacophony emanating from these devices and become inured to the sound. Hospitals face overwhelming noise and false positives from their patient telemetry devices, resulting in hostile work environments and elevating employee attrition. The following are just a few examples of the many articles and papers relating to the topic of alarm fatigue:
Alarm fatigue has caused improper deaths due to medical personnel ignoring critical alarms.
- John Hopkins report – “Using Data to Drive Alarm System Improvement Efforts” :
- “In hospitals today, we have too many alarming devices. The alarm parameters are not set to actionable levels, and the alarm thresholds are set too tight. Monitor alarm systems are very sensitive and unlikely to miss a true event; however, this results in too many false positives. We have moved to large clinical units with unclear alarm system accountability; private rooms with doors closed that make it hard to hear alarm signals; and duplicate alarm conditions which desensitize staff.”
- AAMI article – “Monitor Alarm Fatigue: An integrative Review”:
- “Alarm fatigue, the lack of response due to excessive numbers of alarms resulting in sensory overload and desensitization, is a national problem. From 2005 through 2008, the U.S. Food and Drug Administration (FDA) Manufacturer and User Facility Device Experience (MAUDE) database received 566 reports of patient deaths related to monitoring device alarms. A four-month review of the MAUDE database between March 1, 2010, and June 30, 2010, revealed 73 alarm-related deaths with 33 attributed to physiologic monitors.”
- “The ECRI Institute, a nonprofit organization that uses applied scientific research in healthcare to establish best practices for improving patient care, publishes an annual top ten technology hazards list. “Alarm hazards” is the number one health technology hazard for 2012. Such hazards include inappropriate alarm modification, alarm fatigue, modifying alarms without restoring them to their original settings, and improperly relaying alarm signals to the appropriate person. The problem of excessive alarms resulting in alarm fatigue has been reported in research literature for many years. Studies have indicated that the presence of false and/or clinically insignificant alarms ranges from 80%–99%.”
- American Association of Critical Care Nurses (AACN) article – “Contribution of Electrocardiographic Accelerated Ventricular Rhythm Alarms to Alarm Fatigue”:
- “Excessive clinical alarms can cause “alarm fatigue,” in which nurses become desensitized to alarms, delay their response to the alarms, and in extreme cases turn the alarms off, all of which may result in patient harm due to missed true emergencies. The Joint Commission reported that 98 alarm-related events occurred between 2009 and 2013, with 80 of them resulting in death. The problem of alarm fatigue highlights not only the large volume of clinical alarms that clinicians must attend to (eg, electrocardiographic [ECG], vital signs, ventilators, intravenous pumps), but also the ongoing need for better clinical alarm management and questions about the clinical relevance of alarms to patient care. For example, is every true alarm clinically actionable, and does it improve patient outcomes and/or save lives?”
Imagine yourself in an ICU, trying to recover from major surgery or trauma.
As you lie in your bed trying to rest, you hear another loud beep every few minutes, destroying your ability to sleep. Imagine that it is your loved one attached to these machines while you sit by their bedside, and you keep hearing these loud and raucous alarms that could mean that something is seriously wrong but, in the vast majority of times, means nothing. What would you say if you knew that eighty to ninety-nine percent of those alarms are false positives? What would you say if you knew that everyone in the ICU hears hundreds of false alarms per day per patient? When considering a typical ICU of twenty beds, the noise emitted by those vital signs devices is a scourge.
This situation is especially striking considering how long clinical alarm fatigue has tormented clinicians, patients, and their caregivers.
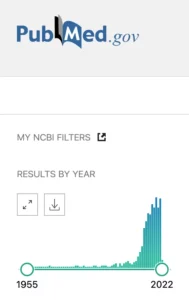
A search of the National Library of Medicine for “Alarm Fatigue” revealed 492 papers written from 1955 to the present day, with the overwhelming majority published in the last ten years.
You may then ask, “Why hasn’t this issue been solved by the vital signs device manufacturers such as GE Healthcare, Philips Healthcare, Medtronic, Masimo, and others? That’s a great question — device manufacturers are always intent on improving their devices with the next version of the firmware, which is right around the corner, being the ones to fix this problem generated by their devices. The alarm fatigue default thresholds are far too sensitive, which is the root cause of this problem.
Combine that with difficult-to-use user interfaces and a big-data crisis overwhelming clinicians’ ability to process, and you get the status quo. The device manufacturers do not have the expertise in AI-driven alert management and routing that the CalmWave team has developed over the years. Their approach is to try to make their devices more “intelligent” and add ever more features, most of which go unused. Our approach is to make the network of vital signs devices, as a whole, smarter. We believe the network approach is a much better solution, as handling a single alert outside the context of the other alarms/signals coming from the patient is insufficient. Solving the scourge of alarm fatigue requires analyzing all signals in a holistic fashion regardless of device vendor.
I’ve worked on alarm fatigue for many years, and we’ve solved it in Enterprise IT Operations at scale for Fortune 100 companies. While there are differences between the two domains of Enterprise IT and Healthcare, the similarities are striking. Our mission at CalmWave is to solve this terrible problem of alarm fatigue for clinicians, patients, and caregivers as the first step in building our Operations Health platform focused on improving nurse retention and hospital maturity. If you think creating quiet ICUs that only generate annunciated alarms that are actionable is a worthwhile goal, contact us at hello@calmwave.ai for more information.
Sources:
Drew BJ, Harris P, Zègre-Hemsey JK, et al. Insights into the problem of alarm fatigue with physiologic monitor devices: a comprehensive observational study of consecutive
Honan L, Funk M, Maynard M, Fahs D, Clark JT, David Y. Nurses’ perspectives on clinical alarms. Am J Crit Care. 2015;24(5):387-395.
Jones K. Alarm fatigue a top patient safety hazard. Can Med Assoc J. 2014;186(3):178.
Joint Commission. Medical device alarm safety in hospitals. Sentinel Event Alert. 2013;50:1-3.